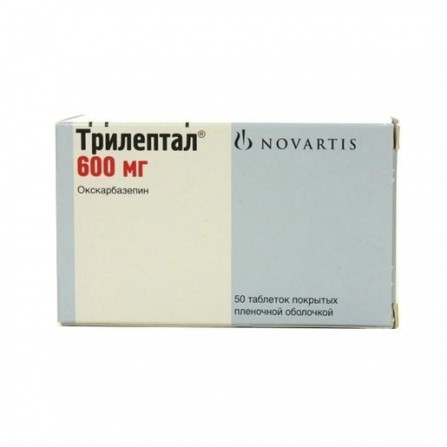
Trileptal pills 600 mg 50 pcs
Condition: New product
1000 Items
Rating:
Be the first to write a review!

More info
Active ingredients
Oxcarbazepine
Release form
Pills
Composition
Active ingredient: Oxcarbazepine (Oxcarbazepine) Active ingredient concentration (mg): 600
Pharmacological effect
Antiepileptic drug. pharmacological activity is primarily due to the action of the metabolite, a monohydroxy derivative (mgp) of oxcarbazepine. The mechanism of action of oxcarbazepine and its metabolite is associated mainly with the blockade of potential-dependent sodium channels, which leads to stabilization of the overexcited neuronal membranes, inhibiting the occurrence of serial neuronal discharges and reducing synaptic conduction of pulses. activated by high membrane potential. no significant interaction with brain neurotransmitters or receptor binding has been noted. In experimental studies, it was shown that oxcarbazepine and its metabolite have a pronounced anticonvulsant effect. The effectiveness of oxcarbazepine in epileptic seizures has been demonstrated both in monotherapy and in the use of oxcarbazepine in combination therapy in children and adults.
Pharmacokinetics
After oral administration, oxcarbazepine is completely absorbed and is largely metabolized to form a pharmacologically active metabolite, a 10-monohydroxy derivative. After a single dose of oxcarbazepine, depending on the dosage form used, the Cmax of the metabolite in the blood plasma is 24.9-34 μmol / l, the average time to achieve it is about 4.5-6 hours. In pharmacokinetic studies it was shown that 2% of oxcarbazepine is detected in the blood plasma and 70% of IHL; the remainder is accounted for by secondary metabolites rapidly evolving from blood plasma. The binding of the metabolite to plasma proteins, mainly albumin, is about 40%. In the therapeutic range, the degree of binding does not depend on the concentration of the drug in the serum. Oxcarbazepine and MHP do not bind to the α1-acid glycoprotein. The seeming Vd - 49 l. Css MHD in plasma is achieved for 2-3 days while taking oxcarbazepine 2 times / day.In equilibrium, the pharmacokinetic parameters of MHD are linear and dose-dependent in the range of daily doses of 300 mg to 2400 mg. Oxcarbazepine is rapidly metabolized by cytosolic enzymes of the liver to the pharmacologically active metabolite of MHP, which is further glucuronized. Minor amounts of IHD (about 4% of the dose) are oxidized to form an inactive metabolite - 10, 11-dihydroxy derivative (BPH). Oxcarbazepine is excreted as metabolites mainly by the kidneys (95%), less than 1% is excreted unchanged. Approximately 80% of excreted metabolites are IHP, of which 49% are glucuronides and 27% are unchanged IHP. BPH is excreted unchanged (about 3%), oxcarbazepine conjugates are 13%. About 4% of the dose is excreted with feces. Oxcarbazepine is rapidly excreted from blood plasma, the apparent T1 / 2 is 1.3–2.3 h. The apparent T1 / 2 MHP averages 9.3 ± 1.8 h. There is a linear relationship between the renal clearance of IHD and creatinine clearance. With CC less than 30 ml / min, after a single dose, 300 mg of oxcarbazepine T1 / 2 IHD is increased to 19 hours, and AUC is doubled. The weight gain of the IHD corrected in children decreases with increasing age and body weight, approaching adult clearance. Body weight adjusted clearance in children aged 1 month to 4 years is 93% higher than in adults. As a result, it is assumed that the AUC of IHL in children of this age group will be 2 times less than that in adults when using the same dose (when adjusted for body weight). Body weight adjusted clearance in children aged 4 to 12 years old is 43% higher than in adults. The estimated AUC of IHD in children of this age group is 2/3 of that in adults with the same doses (when adjusted for body weight). It is assumed that in children aged 13 years and older due to an increase in body weight, the clearance of IHD, adjusted for body weight, corresponds to the clearance of IHD in adults. After receiving oxcarbazepine in a single dose of 300 mg or many times in a dose of 600 mg / day in healthy volunteers aged 60–82 years Сmax in plasma and AUC values for IHL were 30–60% higher compared with the same indicators in young volunteers (18–32 years), which is associated with an age-related decrease in CC. In pregnant women a series of physiological changes occur that may lead to a gradual decrease in the level of IHD in the blood plasma during pregnancy.
Indications
Simple and complex partial epileptic seizures with or without secondary generalization in adults and children aged 1 month and older. Generalized tonic-clonic epileptic seizures in adults and children aged 2 years and older.
Contraindications
Children's age up to 3 years; hypersensitivity to oxcarbazepine.
Precautionary measures
Keep out of the reach of children.
Use during pregnancy and lactation
Experience with pregnancy is limited. Available reports suggest a possible association of oxcarbazepine in pregnancy with the development of congenital defects (such as wolf mouth). In experimental studies with the use of oxcarbazepine in toxic doses, an increase in fetal mortality was observed, as well as a slowdown and impaired development and growth of the fetus. If the patient is planning to become pregnant or become pregnant during the administration of oxcarbazepine, as well as when a question arises about the use of oxcarbazepine during pregnancy, it is necessary to carefully compare the expected benefits of therapy and the possible risk to the fetus, especially in the first trimester of pregnancy. sufficient clinical efficacy in women of childbearing age, oxcarbazepine should be used as monotherapy. In pregnancy should not interrupt effective antiepileptic treatment, since the progression of the disease can have a negative effect on the mother and the fetus. It is known that during pregnancy, folic acid deficiency develops. Antiepileptic drugs may exacerbate this deficiency, which is one of the possible causes of impaired fetal development, therefore additional supplementation with folic acid is recommended. blood. To achieve maximum control of the symptoms of the disease, it is necessary to regularly evaluate the clinical effect of oxcarbazepine and determine the concentration of the metabolite in the blood plasma.It is also recommended to determine the concentration of MHD in the blood plasma in the postpartum period, especially if the dose of oxcarbazepine was increased during pregnancy. There are reports that the use of antiepileptic drugs during pregnancy can lead to increased bleeding in the newborn. As a precautionary measure, vitamin K1 is recommended in the last few weeks of pregnancy, as well as to newborns whose mothers received oxcarbazepine. Oxcarbazepine and IHP penetrate the placental barrier and are excreted in breast milk. The ratio of concentrations in milk and plasma was 0.5 for both substances. Since the effect on newborns of oxcarbazepine and MHDs that are received with mother's milk is unknown, do not use oxcarbazepine during breastfeeding.
Dosage and administration
Is inside. The initial dose is 8-10 mg / kg body weight / day. Further, the dose is adjusted depending on the treatment regimen, the patient's age, the effectiveness of treatment, and renal function. For patients with impaired renal function (QC less than 30 ml / min), an initial dose adjustment and dosing regimen are required.
Side effects
Most often (≥ 10%): drowsiness, headache, dizziness, diplopia, nausea, vomiting, feeling tired. On the hemopoietic system: sometimes leukopenia; very rarely - suppression of bone marrow hematopoiesis, agranulocytosis, aplastic anemia, neutropenia, pancytopenia, thrombocytopenia. On the immune system: very rarely - hypersensitivity reactions accompanied by fever and rash (including organ disorder). With the development of hypersensitivity reactions, damage to the circulatory and lymphatic systems (eosinophilia, thrombocytopenia, lymphadenopathy, splenomegaly), muscles and joints (myalgia, swelling in the joints, arthralgia), nervous system (encephalopathy), kidneys (proteinuria, interstitial nephritis, renal failure ), lungs (shortness of breath, pulmonary edema, bronchospasm, interstitial inflammation), abnormal liver function indices, angioedema, anaphylactic reactions. On the metabolic side: often gi onatriemiya; very rarely - clinically significant hyponatremia (sodium concentration less than 125 mmol / l - usuallyduring the first 3 months of drug therapy; in some patients - more than 1 g after the start of treatment), leading to the development of such manifestations and symptoms as convulsive seizures, confusion, decreased consciousness, encephalopathy, visual impairment (including blurred vision), nausea, vomiting, folic acid deficiency; very rarely - hypothyroidism. On the CNS side: very often - drowsiness, headache, dizziness; often - ataxia, tremor, nystagmus, impaired attention, amnesia; confusion, depression, apathy, agitation, emotional lability. On the part of the sense organs: very often - diplopia; often - visual disturbances, blurred vision, vertigo. From the cardiovascular system: very rarely - arrhythmias, AV-blockade, arterial hypertension. From the alimentary system: very often - nausea, vomiting; often - diarrhea, constipation, abdominal pain; sometimes - increased activity of liver enzymes, increasing the concentration of alkaline phosphatase in the blood; very rarely - pancreatitis and / or increased levels of lipase and / or amylase, hepatitis. Dermatological reactions: often - rash, alopecia, acne. Allergic reactions: sometimes - urticaria; very rarely - angioedema, Stevens-Johnson syndrome, toxic epidermal necrolysis (Lyell's syndrome), erythema multiforme. Other: very often - feeling tired; often - asthenia; very rarely - systemic lupus erythematosus. In children under 4 years of age: very often (11%) - drowsiness; often (≥1% –10% less) - ataxia, irritability, vomiting, lethargy, fatigue, nystagmus, tremor, loss of appetite, increased uric acid concentration in the blood.
Interaction with other drugs
Oxcarbazepine and its pharmacologically active metabolite MHP are inhibitors of cytochrome CYP2C19. Therefore, when using oxcarbazepine in high doses, it is possible to drug interaction with drugs metabolized by CYP2C19 (phenobarbital, phenytoin). For some patients, it may be necessary to reduce the dose of drugs - substrates of CYP2C19. It was shown that the Omsk is in charge of the Chechen Republic; calcium antagonists, oral contraceptives, and antiepileptic drugs (for example, carbamazepine).With simultaneous use with oxcarbazepine, it is also possible to decrease plasma concentrations and other drugs that are substrates of CYP3A4 and CYP3A5 enzymes (for example, drugs of the immunosuppressant group - cyclosporine). Since in vitro IHL is a weak inducer of UDP-glucuronyl transferase and, therefore, it is unlikely that in vivo, it is able to affect the metabolism of drugs excreted in the form of conjugates with glucuronic acid (for example, valproic acid and lamotrigine). But, taking into account even the weak inducing ability of oxcarbazepine and IHP, it may be necessary to increase the doses of concurrently used drugs metabolized with CYP3A4 or UDP-glucuronyltransferase. If oxcarbazepine is withdrawn, a reduction in the dose of these drugs may be required. In vitro, studies confirmed the weak inducing capacity of oxcarbazepine and IHP in relation to the isoenzymes of the subsystems of the CYP2B and CYP3A4 enzymes. The inductive effect of oxcarbazepine and MHP on other CYP isoenzymes is unknown. The concentration of phenytoin in plasma increases to 40% with simultaneous use of oxcarbazepine at a dose of 1200 mg / day and above. Therefore, when using oxcarbazepine in such doses, it may be necessary to reduce the dose of phenytoin. Increasing the serum concentration of phenobarbital while using oxcarbazepine slightly (15%). Simultaneous administration of strong inducers of cytochrome P450 isoenzymes (i.e., carbamazepine, phenytoin and phenobarbital isoenzymes for reducing cytochrome P450 isoenzymes (IGP, phenytoin, phenytoin and phenobarbital) to reduce cytochrome P450 isotopes. blood plasma (by 29–40%). Proven interaction of oxcarbazepine with ethinyl estradiol and levonorgestrel. The mean AUC values for them decreased by 48–52% and 35–52%, respectively. Studies on the interaction of oxcarbazepine with other oral or implantable contraceptives have not been conducted. Thus, the simultaneous use of oxcarbazepine and hormonal contraceptives can lead to a decrease in the effectiveness of the latter. Simultaneous use of oxcarbazepine and felodipine can lead to a decrease in the AUC value of felodipine by 28%, although plasma concentrations remain within the therapeutic range. On the other hand, while using verapamil may reduce the concentration of IHD in the serum by 20%.Such a decrease has no clinical significance. Cimetidine, erythromycin, dextropropoxyphene do not affect the pharmacokinetic parameters of MHD; Viloxazin has little effect on plasma IHP concentration (IHP concentration increases by 10% after repeated co-administration). No interaction with warfarin is noted when taking both single and multiple doses of oxcarbazepine. Oxarbazepine may increase the sedative effect of ethanol.
special instructions
Use with caution in patients with known hypersensitivity to carbamazepine, because In this group of patients, hypersensitivity reactions to oxcarbazepine may develop in approximately 25–30% of cases. In patients with no history of indications of hypersensitivity to carbamazepine, hypersensitivity reactions to oxcarbazepine, including multiple organ dysfunctions, may also develop. In the case of the development of immediate-type hypersensitivity reactions, oxcarbazepine should be immediately discontinued to prescribe an alternative therapy. Use with caution in patients with severely impaired liver function. In patients with impaired renal function and with low serum sodium concentration, or in patients receiving concomitant medication, conducive to the removal of sodium from the body (diuretics, drugs that affect the secretion of ADH), before the start of therapy with oxcarbazepine should determine the concentration uw sodium in the blood serum. In the future, the concentration of sodium in the serum should be monitored 2 weeks after the start of therapy and then monthly for 3 months or as needed. Special attention should be given to these risk factors in elderly patients. If necessary, the appointment of diuretics and other drugs that reduce the concentration of sodium in the serum, patients receiving oxcarbazepine should follow the same recommendations. With the appearance of clinical symptoms that allow to suspect hyponatremia, the concentration of sodium in the blood serum should be measured. For the remaining patients, the measurement of serum sodium concentration can be performed during routine blood tests. When symptoms of pronounced inhibition of bone marrow hematopoiesis develop, it is necessary to consider abolishing oxcarbazepine. Patients who received anticonvulsants have rarely experienced suicidal behaviors and thinking.The mechanism of increasing the risk of suicide in this category of patients has not been established. Therefore, at all stages of treatment, careful monitoring of patients receiving oxcarbazepine is necessary. Body weight should be monitored in all patients with heart failure for timely determination of fluid retention. When fluid retention or the progression of symptoms of heart failure should be determined by the concentration of sodium in the serum. In the event of hyponatremia, limit the amount of fluid consumed. When using oxcarbazepine in very rare cases, a violation of cardiac conduction is possible, therefore, during treatment, careful monitoring of patients with previous conduction disorders (AV blockade, arrhythmia) is necessary. When using oxcarbazepine, dermatological reactions were observed in both children and adults, and developed on average 19 days after the start of treatment. There are separate reports of cases of recurrence of skin reactions with resumption of oxcarbazepine. With the development of skin reactions on the background of the use of oxcarbazepine, it is necessary to consider its cancellation and the appointment of another antiepileptic drug. If you suspect that you have hepatitis, you should consider withdrawing oxcarbazepine. Like any other antiepileptic drugs, oxcarbazepine should be gradually canceled due to the risk of an increase in the incidence of seizures .The effect on the ability to drive vehicles and control mechanismsPatients who have dizziness during the background of the use of oxcarbazepine No drowsiness or other disorders of the central nervous system, should not drive or work with mechanisms during the treatment period.