More info
Active ingredients
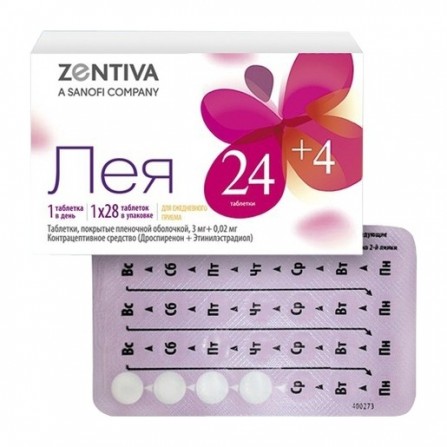
Drospirenone + Ethinyl Estradiol
Release form
Pills
Composition
Tablets, film-coated pink, round, biconvex (24 pieces in a blister). 1 tab. Ethinyl estradiol 20 mcg drospirenone 3 mg. Excipients: lactose monohydrate - 68.18 mg, potassium polacrilin - 4 mg, povidone K30 - 4 mg, magnesium stearate - 0.8 mg. The composition of the film shell: opadry II pink 85F34048 (macrogol 3350 - 0.404 mg, titanium dioxide - 0.496 mg, polyvinyl alcohol - 0.8 mg, talc - 0.296 mg, iron dye red oxide - 0.0036 mg, iron dye yellow oxide - 0.0004 mg) - 2 mg. Tablets, film coated (placebo) white, round, biconvex (4 pieces in a blister). Excipients: lactose monohydrate - 73.4 mg, potassium polacrilin - 1.6 mg, povidone K30 - 4 mg, colloidal silicon dioxide - 0.2 mg, magnesium stearate - 0.8 mg. The composition of the film shell: opadry II white 85F18422 (macrogol 3350 - 0.8 mg, titanium dioxide - 0.5 mg, polyvinyl alcohol - 0.404 mg, talc - 0.296 mg) - 2 mg.
Pharmacological effect
Monophasic combined oral contraceptive (COC), which includes ethinyl estradiol and progestogen drospirenone. The contraceptive effect of the drug Leia is based on the interaction of various factors, of which the most important are the suppression of ovulation and changes in the properties of the cervical secretion, as a result of which it becomes less permeable to spermatozoa. In therapeutic doses, drospirenone also has antiandrogenic and moderate anti-mineralocorticoid properties, which gives drospirenone a pharmacological profile similar to that of natural progesterone. Drospirenone helps to reduce the symptoms of acne (acne), oily skin and hair, prevents weight gain and the appearance of edema associated with estrogen-induced fluid retention, which ensures a very good tolerability of Leia. The positive effects and clinical efficacy of drospirenone in alleviating the symptoms of severe premenstrual syndrome (PMS), such as pronounced psycho-emotional disorders, engorgement of the mammary glands, headache, muscle and joint pain, weight gain, and other symptoms associated with the menstrual cycle. In combination with ethinyl estradiol, drospirenone demonstrates a beneficial effect on the lipid profile, characterized by an increase in the content of HDL in the blood plasma.In women taking COC, the menstrual cycle becomes more regular, less frequent painful menstruation, decreases the intensity of bleeding, which reduces the risk of anemia. In addition, according to epidemiological studies, the use of COC reduces the risk of developing endometrial cancer and ovarian cancer.
Pharmacokinetics
Drospirenone Absorption When administered orally, drospirenone is rapidly and almost completely absorbed. After a single ingestion of Cmax in the blood plasma, equal to about 38 ng / ml, is achieved in approximately 1-2 hours. Bioavailability is 76-85%. Meal does not affect the bioavailability of drospirenone. Distribution After oral administration, the concentration of drospirenone in plasma decreases biphasic, with T1 / 2 in the second phase - 31 hours. Drospirenone binds to plasma albumin and does not bind to sex hormone-binding globulin (SHBG) or corticosteroid-binding globulin (KSG) . Only 3-5% of the total plasma concentration of the substance is present as a free steroid. An ethinyl estradiol-induced increase in SHBG does not affect the binding of drospirenone to plasma proteins. The average apparent Vd is 3.7 ± 1.2 L / kg. Equilibrium concentration. During the cycle treatment, Cssmax of drospirenone in the blood plasma is reached after 8 days of taking the drug and is approximately 70 ng / ml. There was an increase in plasma concentration of drospirenone approximately 2-3 times (due to cumulation), which was caused by the T1 / 2 ratio in the terminal phase and dosing interval. A further increase in the plasma concentration of drospirenone is observed between 1 and 6 cycles of administration, after which no increase in concentration is observed. Metabolism After oral administration, drospirenone is extensively metabolized. Most plasma metabolites are represented by the acidic forms of drospirenone. Withdrawal The rate of metabolic clearance of drospirenone in plasma is 1.5 ± 0.2 ml / min / kg. In unchanged form, drospirenone is excreted only in trace amounts. Metabolites of drospirenone are excreted through the intestine and kidneys in a ratio of approximately 1.2: 1.4. T1 / 2 with excretion of metabolites is approximately 24 hours. Pharmacokinetics in special clinical situations Patients with renal insufficiency.Css of drospirenone in plasma in women with mild renal insufficiency (CK 50-80 ml / min) were comparable to those in women with normal renal function (CK> 80 ml / min). In women with moderately severe renal failure (CK 30–50 ml / min), plasma concentration of drospirenone was on average 37% higher than in women with normal renal function. Drospirenone treatment was well tolerated in all groups. The intake of drospirenone did not have a clinically significant effect on the concentration of potassium in the blood plasma. Pharmacokinetics for severe renal failure has not been studied. Patients with liver failure Drospirenone is well tolerated by patients with mild to moderate hepatic insufficiency (Child-Pugh grade B). Pharmacokinetics for severe hepatic insufficiency has not been studied. Ethinyl estradiol Absorption After oral administration, ethinyl estradiol is rapidly and completely absorbed. The peak plasma concentration after a single oral administration is reached after 1-2 hours and is about 33 pg / ml. The absolute bioavailability as a result of presystemic conjugation and metabolism of the first passage is approximately 60%. Concomitant food intake reduces the bioavailability of ethinyl estradiol in about 25% of those examined, while other patients did not show similar changes. Distribution The concentration of ethinyl estradiol in blood plasma decreases biphasic; T1 / 2 is approximately 24 hours. Ethinyl estradiol is largely and not specifically bound to plasma albumin (approximately 98.5%) and causes an increase in plasma SHG concentrations. The average apparent Vd is about 5 l / kg. Metabolism Ethinyl estradiol undergoes systemic conjugation in the mucosa of the small intestine and in the liver. Ethinyl estradiol is primarily metabolized by aromatic hydroxylation, with the formation of various hydroxylated and methylated metabolites, presented both as free metabolites and as conjugates with glucuronic and sulfuric acids. Ethinyl estradiol is fully metabolized; metabolic clearance rate is about 5 ml / min / kg. Withdrawal Ethinyl estradiol is practically not excreted unchanged.Ethinyl estradiol metabolites are excreted through the kidneys and intestines at a ratio of 4: 6; T1 / 2 is about 1 day. Equilibrium concentration The state of equilibrium concentration is reached during the second half of the drug intake cycle, and the concentration of ethinyl estradiol in the blood plasma increases approximately 1.4-2.1 times. Preclinical safety data Preclinical data obtained in the course of standard studies to identify toxicity with repeated doses of the drug, as well as genotoxicity, carcinogenic potential and toxicity to the reproductive system, do not indicate the presence of a particular risk to humans. Nevertheless, it should be remembered that sex hormones can promote the growth of certain hormone-dependent tissues and tumors.
Indications
- contraception; - contraception and treatment of moderate acne (acne vulgaris); - contraception and treatment of severe premenstrual syndrome (PMS).
Contraindications
Leia is contraindicated in the presence of any of the conditions listed below; If any of these conditions arise for the first time during the treatment of COCs, they should be stopped immediately. - thrombosis (venous and arterial) and thromboembolism at present or in history (including deep vein thrombosis, thromboembolism of the pulmonary artery, myocardial infarction), cerebrovascular disorders (including in history); - conditions preceding thrombosis (including transient ischemic attacks, angina pectoris) now or in history; - hereditary or acquired susceptibility to the development of venous or arterial thrombosis, such as resistance to activated protein C, deficiency of antithrombin III, deficiency of protein C, deficiency of protein S, hyperhomocysteinemia and antiphospholipid antibodies (antibodies to cardiolipin, lupus anticoagulant); - migraine with focal neurological symptoms at present or in history; - multiple or pronounced risk factors for venous or arterial thrombosis, including complicated lesions of the valvular apparatus of the heart, atrial fibrillation; diseases of cerebral vessels or coronary arteries; uncontrolled arterial hypertension; severe dyslipoproteinemia, diabetes mellitus with vascular complications,serious surgical intervention with prolonged immobilization; smoking over the age of 35; obesity with a BMI of more than 30 kg / m2; extensive injury; - liver failure, severe liver disease (until normalization of liver function indicators); - liver tumors (benign or malignant), incl. in the anamnesis; - severe renal failure, acute renal failure; - adrenal insufficiency; - pancreatitis, incl. in history if associated with the presence of severe triglyceridemia; - identified hormone-dependent malignant diseases (including genitals or mammary glands) or suspicion of them; - bleeding from the vagina of unspecified etiology; - pregnancy or suspicion of it; - breastfeeding period; - lactose intolerance, lactase deficiency, glucose-galactose malabsorption (lactose monohydrate is included); - Hypersensitivity to any component of the drug Leia. With caution If a patient has any of the conditions / risk factors listed below, carefully consider the potential risk and the expected benefits of using COC, including Leia. - risk factors for thrombosis and thromboembolism: smoking, thrombosis (including history), myocardial infarction, or cerebral circulation at a young age in one of the closest relatives; obesity with a BMI less than 30 kg / m2; dyslipoproteinemia; controlled arterial hypertension; migraine without focal neurological symptoms; valvular disease without complications; heart rhythm disorder; - other diseases in which there may be violations of the peripheral circulation: diabetes mellitus; systemic lupus erythematosus; hemolytic uremic syndrome; Crohn's disease and ulcerative colitis; sickle cell anemia; as well as phlebitis of the superficial veins; - hereditary angioedema; - hypertriglyceridemia; - liver disease; - Diseases that first arose or aggravated during pregnancy or against the background of previous intake of sex hormones (for example, jaundice, cholestasis, cholelithiasis, otosclerosis with impairment of hearing, porphyria, herpes of pregnant women, Sydengam's chorea); - postpartum period.
Use during pregnancy and lactation
Leia drug is contraindicated for use in pregnancy.If pregnancy occurs while taking the drug Leia, you must immediately stop taking it. Conducted epidemiological studies did not reveal an increase in the risk of birth defects in children born to mothers who took COCs before pregnancy, nor a teratogenic effect when COCs were taken carelessly in early pregnancy. Available data on the use of the drug Leia during pregnancy are too limited and do not allow to conclude that it has a negative effect on pregnancy or on the health of the fetus or newborn. Leia is contraindicated during breastfeeding. COCs can reduce the amount of breast milk and change its quality. A small amount of sex hormones and / or their metabolites can penetrate into breast milk and, possibly, can have an effect on the baby.
Dosage and administration
Leia is intended to be taken daily for 28 days without interruption, approximately at the same time, with a small amount of water, in the order indicated on the blister package. Taking the pills from the new package starts the day after taking the last tablet from the previous package. How to take the drug Leia If you have not taken any hormonal contraceptives in the previous month Taking the drug Leia begins on the first day of the menstrual cycle (ie, on the first day of the menstrual bleeding). It is allowed to start taking on the 2-5 day of the menstrual cycle, but in this case it is recommended to additionally use a barrier method of contraception during the first 7 days of taking the pills from the new package. Bleeding "cancellation", as a rule, begins on the 2-3rd day after the start of taking inactive pills and may not end before the start of taking the pills from a new package. When switching from other combined oral contraceptives (COC, vaginal ring or transdermal patch) It is preferable to start taking the drug Leia the next day after taking the last active tablet from the previous package, but in no case later than the next day after the usual 7-day break (for drugs containing 21 active pills) or after taking the last inactive tablet (for drugs containing 28 pills per pack).Leia should be taken on the day of removal of the vaginal ring or contraceptive patch, but no later than the day when a new patch is to be inserted or a new patch is stuck. When switching from contraceptives containing only gestagens ("mini-pili", injection forms, implant or intrauterine contraceptive), a woman can switch from "mini-pili" to taking Ley on any day (without a break) from an implant or intrauterine therapy progestogen-releasing agent - on the day of its removal, with an injection contraceptive - on the day when the next injection should be given. In all cases, you must use an additional barrier method of contraception during the first 7 days of taking pills. After an abortion in the first trimester of pregnancy. A woman can start taking the drug Leia from the first day after the abortion. Subject to this condition, the woman does not need additional contraceptive measures. After childbirth or abortion in the second trimester of pregnancy It is recommended to start taking the drug Leia on days 21-28 after giving birth, in the absence of breastfeeding, or abortion in the second trimester of pregnancy. If reception is started later, you must use an additional barrier method of contraception during the first 7 days of taking the pills. However, if a woman has already lived sexually, before pregnancy begins, Leia should be excluded from pregnancy. Taking the missed pills Skipping inactive pills can be ignored. However, they should be thrown away in order not to accidentally extend the intake of inactive pills. The following recommendations apply only to skipping active pills: - if a delay in taking the drug was less than 24 hours, the contraceptive protection is not reduced. A woman should take the missed pill as soon as possible and take the next one at the usual time. - If the delay in taking the pills was more than 24 hours, contraceptive protection may be reduced. The more pills are missed, and the closer the pill passes to the inactive pill intake phase, the higher the chance of pregnancy. The following basic rules can be followed: - the drug should never be interrupted for more than 7 days (the recommended interval for taking inactive pills is 4 days); - to achieve adequate suppression of the hypothalamic-pituitary-ovarian system requires 7 days of continuous administration of pills.Thus, if the delay in taking active pills was more than 24 hours, we can recommend the following: From the 1st to the 7th day, the Woman should take the last missed pill as soon as she remembers, even if it means taking two pills at the same time. She continues to take the following pills at the usual time. In addition, over the next 7 days, you must additionally use a barrier method of contraception (for example, a condom). If sexual intercourse occurred within 7 days before the tablet is missed, the possibility of pregnancy should be considered. From the 8th to the 14th day, a woman should take the last missed pill as soon as she remembers it, even if it means taking two pills at the same time. The following pills should be taken at the usual time. Provided that the woman took the pill correctly for the 7 days preceding the first missed pill, there is no need to use additional contraceptive measures. Otherwise, as well as skipping two or more pills, you must additionally use barrier methods of contraception (for example, a condom) for 7 days. From the 15th to the 24th day The risk of reducing the reliability is inevitable due to the approaching phase of taking inactive pills. A woman should strictly adhere to one of the following two options. However, if in the 7 days preceding the first missed pill, all the pills were taken correctly, there is no need to use additional contraceptive methods. Otherwise, she needs to use the first of the following schemes and additionally use a barrier method of contraception (for example, a condom) within 7 days. Option 1: a woman should take the last missed pill as soon as possible, as soon as she remembers (even if it means taking two pills at the same time). The following pills are taken at the usual time until the active pills in the package run out. Four inactive pills should be thrown away and immediately start taking the pills from the next package. Bleeding "cancellation" is unlikely until the active pills in the second pack run out, but there may be "spotting" discharge and "breakthrough" bleeding while taking the pills.Option 2: a woman can also interrupt the intake of pills from the current package. Then she should take a break of no more than 4 days, including the days of skipping the pills, and then start taking pills from a new pack. If a woman missed active pills, and while taking inactive pills, the "cancellation" bleeding did not occur, it is necessary to exclude pregnancy. Recommendations for gastrointestinal disorders In severe gastrointestinal disorders, the absorption of the drug may be incomplete, therefore additional contraceptive measures should be taken. If vomiting occurs within 4 hours after taking the active pill, refer to the recommendations for skipping pills. If a woman does not want to change her usual regimen and postpone the onset of menstruation to another day of the week, an additional active pill should be taken from another package. Changing the day of the onset of menstrual bleeding In order to delay the onset of menstrual bleeding, a woman should continue taking the pills from the next pack, skipping the inactive pills from the current pack. Thus, the cycle can be extended, if desired, for any period until the active pills from the second package run out. While taking the pills from the second package, a woman may experience "spotting" discharge or "breakthrough" uterine bleeding. Regular intake of the drug Leia is resumed after the end of the phase of taking inactive pills. In order to postpone the day of the onset of menstrual bleeding to another day of the week, a woman should cut the next phase of inactive pills for the desired number of days. The shorter the interval, the higher the risk that she will not have “withdrawal” bleeding and in the future there will be “spotting” spotting and “breakthrough” bleeding while taking the second package (just as if she would like to delay the onset of a menstrual bleeding). How to delay bleeding "cancellation" In order to delay the onset of menstruation, a woman should switch to taking pills from a new pack of Leia, skipping taking placebo pills. Such a prolongation of the cycle can be continued until the active pills of the second package run out.During this extension, a woman may experience "breakthrough" bleeding or spotting. In the future, you should resume regular use of the drug Leia after the usual interval without taking the pills, which is 7 days. To postpone the onset of menstruation to another day, more suitable for a woman’s usual schedule, it is possible to reduce the second phase of taking placebo pills for as many days as necessary. The shorter this phase, the higher the risk that the "withdrawal" bleeding does not develop, and that there will be "breakthrough" bleeding or bleeding during the taking of pills from the second package (as well as a postpone menstruation). Special patient categories Children and adolescents: Leia's drug is indicated only after the onset of menarche. The available data do not suggest dose adjustment in this group of patients. Elderly patients: not applicable. Leia's drug is not indicated after menopause. Leia's drug is contraindicated in women with severe liver disease until liver function rates return to normal. Leia is contraindicated in women with severe renal insufficiency or acute renal failure.
Side effects
Clinical research data The incidence of adverse reactions is presented according to the classification (MedDRA): very often (> 10%), often (1% <10%), infrequently (0.1% <1%), rarely (0.01% <0.1%) , very rarely (<0.01%), the frequency is unknown (it is not possible to determine the frequency of occurrence from the available data). Infectious and parasitic diseases: infrequently - candidiasis of the oral mucosa, vaginal candidiasis, herpes simplex. On the part of the immune system: rarely - allergic reactions, rarely - bronchial asthma; frequency is unknown - hypersensitivity reactions. From the side of blood and lymphatic system: rarely - anemia, thrombocytopenia. Mental disorders: often - emotional lability; infrequently - depression, nervousness, sleep disorder; rarely - anorgasmia. From the nervous system: often - headache; infrequently - paresthesia, dizziness, migraine; rarely - tremor. On the part of the organ of vision: infrequently - conjunctivitis, dry eye syndrome, visual impairment. On the part of the organ of hearing and labyrinth disturbances: rarely - hearing loss.Since the cardiovascular system: infrequently - extrasystoles, tachycardia, pulmonary thromboembolism, increased blood pressure, lower blood pressure, varicose veins; rarely - arterial and venous thromboembolism, syncope. On the part of the respiratory system, organs of the chest and mediastinum: pharyngitis. On the part of the digestive system: often - nausea; infrequently - vomiting, gastroenteritis, diarrhea; rarely - constipation, abdominal pain, bloating. On the part of the liver and biliary tract: rarely - cholecystitis. On the part of the skin and subcutaneous tissues: infrequently - pruritus, rash, seborrhea, acne; rarely - alopecia, dry skin, eczema, photodermatitis, acneform dermatosis, hypertrichosis, stretch marks, erythema nodosum, erythema multiforme. From the musculoskeletal and connective tissue: infrequently - pain in the neck, limbs, lumbar region; muscle cramps. On the part of the kidneys and urinary tract: infrequently - cystitis. On the part of the genital organs and mammary gland: often - pain in the mammary glands, engorgement of the mammary glands, metrorrhagia, absence of menstrual-like bleeding; infrequently - mammary neoplasms, galactorrhea, ovarian cyst, "hot flashes", leucorrhea, vaginal mucosa dryness, pain in the pelvic region, changes in Pap smear results, decreased libido, breast enlargement, painful menstrual bleeding, poor menstrual-like bleeding; rarely - fibrocystic mastopathy, vaginitis, cervical polyp, cervical neoplasia, endometrial atrophy, heavy menstrual-like bleeding, dyspareunia, postcoital bleeding, "withdrawal" bleeding, an increase in the size of the uterus. On the part of the endocrine system: very rarely - changes in glucose tolerance or the effect on insulin resistance. General disorders and disorders at the injection site: often - weight gain; infrequently - increased appetite, weight loss, anorexia, edema, asthenia, excessive feeling of thirst, sweating. Laboratory and instrumental data: infrequently - hyperkalemia, hyponatremia. Post-marketing data The following serious adverse reactions have been reported with an unknown frequency in women taking COC: venous thromboembolic complications, arterial thromboembolic complications, increased blood pressure, liver tumors.The connection with taking COCs is not convincing when the following diseases appear or worsen: Crohn's disease, ulcerative colitis, epilepsy, uterine myoma, porphyria, systemic lupus erythematosus, pregnant herpes, Sydengham's chorea, hemolytic uremic syndrome, cholestatic jaundice, chloasma. Acute and chronic liver dysfunction may require discontinuation of COC until liver function markers return to normal. In women with hereditary angioedema, exogenous estrogens can cause the manifestation of the disease or its exacerbation. The frequency of breast cancer diagnostics among women taking COCs is slightly increased, although a causal relationship with COC use has not been established.
Overdose
Until now, there has not been a single case of an overdose of Leia. Given the clinical experience with COCs, in the event of an overdose of the drug, the following symptoms may be observed: nausea, vomiting, "bloody" spotting or metrorrhagia. There is no antidote, symptomatic treatment.
Interaction with other drugs
The interaction of oral contraceptives with other drugs can lead to "breakthrough" bleeding and / or a decrease in contraceptive reliability. Women taking these drugs should temporarily use barrier methods of contraception in addition to taking the drug Leia or choose another method of contraception. The use of drugs that induce liver microsomal enzymes, can lead to an increase in the clearance of sex hormones. Such drugs include: phenytoin, barbiturates, primidone, carbamazepine, rifampicin; there are also assumptions regarding oxcarbazepine, topiramate, felbamate, griseofulvin, and preparations containing St. John's wort. HIV proteases (eg, ritonavir) and non-nucleoside reverse transcriptase inhibitors (eg, nevirapine), and combinations thereof, also have the potential to affect hepatic metabolism. According to individual studies, some antibiotics (for example, penicillins and tetracycline) can reduce the enterohepatic recirculation of estrogen, thereby lowering the concentration of ethinyl estradiol.During the intake of drugs that affect microsomal enzymes, and within 28 days after their withdrawal, a barrier method of contraception should be additionally used. During the reception of antibiotics (such as ampicillins and tetracyclines) and within 7 days after their cancellation, you should additionally use a barrier method of contraception. If active (pink) pills run out during these 7 days of using a barrier method of contraception, then you should skip the placebo pills (white) from the current package and start taking the pills from the next package of Leia. The main metabolites of drospirenone are formed in plasma without the participation of isoenzymes of the cytochrome P450 system. Therefore, the effect of cytochrome P450 isoenzyme inhibitors on the metabolism of drospirenone is unlikely. COCs can affect the metabolism of other drugs, which leads to an increase (for example, cyclosporine) or a decrease (for example, lamotrigine) of their concentration in plasma and tissues. Based on in vitro interaction studies, as well as in vivo studies in female volunteers taking omeprazole, simvastatin and midazolam as markers, it can be concluded that the effect of drospirenone at a dose of 3 mg on the metabolism of other drugs is unlikely. There is a theoretical possibility of increasing the concentration of potassium in the blood plasma in women who receive Leia simultaneously with other drugs that can increase the concentration of potassium in the blood plasma. These drugs include ACE inhibitors, angiotensin II receptor antagonists, some nonsteroidal anti-inflammatory drugs, potassium-saving diuretics, and aldosterone antagonists. However, in studies evaluating the interaction of drospirenone with ACE inhibitors or indomethacin, there was no significant difference between the plasma concentration of potassium in comparison with placebo. However, in women taking drugs that can increase the concentration of potassium in the blood plasma, it is recommended to determine the concentration of potassium in the blood plasma during the first cycle of taking the drug Leia. To determine possible interactions with drugs taken at the same time as Leia, you should read the instructions for use of these drugs.
special instructions
If any of the conditions / risk factors listed below are present, then the potential risk and the expected benefits of using COCs in each individual case should be carefully weighed and discussed with the patient before taking the drug. In the event of a worsening, aggravation, or first manifestation of any of these conditions or risk factors, the woman should consult with her physician, who may decide to discontinue the drug. Diseases of the cardiovascular system The results of epidemiological studies indicate a relationship between the use of COCs and an increase in the incidence of venous and arterial thrombosis and thromboembolism (such as deep vein thrombosis, pulmonary thromboembolism, myocardial infarction, cerebrovascular disorders) when taking COCs. These diseases are rare. The risk of venous thromboembolism (VTE) is maximum in the first year of taking such drugs. Increased risk is present after the initial use of the COC or the resumption of use of the same or different COCs (after a break between taking the drug in 4 weeks or more), mostly during the first 3 months. The overall risk of VTE in patients taking low-dose COCs (<50 μg of ethinyl estradiol) is 2–3 times higher than in non-pregnant patients who do not take COC, however, this risk remains lower compared with the risk of VTE during pregnancy and