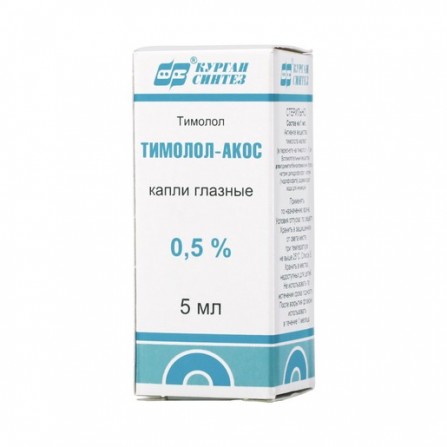
Timolol Solofarm eye drops 0.5% 5ml
Condition: New product
1000 Items
Rating:
Be the first to write a review!

More info
Active ingredients
Timolol
Release form
Drops
Composition
1 ml of the preparation contains: Active substance: taurine - 40 mg. Excipient: water for injection - up to 1 ml.
Pharmacological effect
Nonselective beta-adrenergic receptor blocker without sympathomimetic activity. It does not have significant internal sympathomimetic, directly inhibitory myocardium and local anesthetic (membrane stabilizing) activity. The blockade of beta-adrenoreceptors in the bronchi and bronchioles increases the resistance of the respiratory tract, due to the absence of antagonism to parasympathomimetic activity. Such an effect in patients with asthma or other bronchospastic conditions can be a potential hazard. The blockade of beta-adrenoreceptors reduces cardiac output in both healthy subjects and patients with heart disease. In patients with severely impaired myocardial function, blockade of beta-adrenergic receptors may weaken the stimulating effect of the sympathetic nervous system, which is necessary to maintain adequate heart function. When applied topically in the form of eye drops reduces both normal and increased intraocular pressure by reducing the formation of intraocular fluid. Increased intraocular pressure is a major risk factor in the pathogenesis of development characteristic of glaucoma lesions of the optic nerve and narrowing of the boundaries of the visual fields. Does not affect the width of the pupil and accommodation. The exact mechanism for reducing intraocular pressure due to timolol is not known. According to the data of tonography and fluorometry in humans, timolol, when applied topically, lowers the intraocular pressure by reducing the formation of aqueous humor and a small increase in its outflow. Reducing intraocular pressure, does not affect the accommodation and pupil size, therefore, there is no deterioration in visual acuity; does not reduce the quality of night vision. The effect appears 20 minutes after instillation. The maximum effect is observed after 1-2 hours. The duration of action is 24 hours.
Pharmacokinetics
Timolol quickly penetrates the cornea into the tissue of the eye. After instillation in moisture of the anterior chamber of the eye, the maximum concentration (Cmax) in the blood plasma is reached in 1-2 hours.In small quantities into the systemic circulation by absorption through the conjunctiva, the mucous membranes of the nose and lacrimal tract. Cmax of timolol in plasma is about 0.824 ng / ml and is maintained until the detection threshold for 12 hours. In newborns and young children, Cmax of timolol significantly exceeds Cmax in adult plasma. The half-life (T1⁄2) of timolol is 4.8 h after topical administration. Timolol is metabolized by the CYP2D isoenzyme. Timolol and formed metabolites are mainly excreted by the kidneys.
Indications
Increased intraocular pressure (ophthalmic hypertension), open-angle glaucoma, glaucoma in the active eye and other types of secondary glaucoma, congenital glaucoma (with the ineffectiveness of other means), as an additional means to reduce intraocular pressure in closed-angle glaucoma (in combination with myotics).
Contraindications
Bronchial asthma, sinus bradycardia, II and III degree atrioventricular block without a pacemaker, decompensated chronic heart failure, cardiogenic shock, severe chronic obstructive pulmonary disease, sick sinus syndrome, hypersensitivity to the components of the drug.
Precautionary measures
Cerebrovascular insufficiency, arterial hypotension, diabetes mellitus, hypoglycemia, pulmonary insufficiency, thyrotoxicosis, myasthenia gravis, sinoatrial blockade, impaired peripheral circulation (including Raynaud's syndrome), pregnancy, simultaneous administration of other beta-blockers.
Use during pregnancy and lactation
In pregnancy, use with caution only in the case when the expected therapeutic effect for the mother outweighs the potential risk to the fetus or child. If necessary, the use of the drug during lactation breastfeeding should be discontinued.
Dosage and administration
At the beginning of treatment, 1-2 drops to the affected eye, 2 times a day. If the intraocular pressure with normal use is normalized, the dose should be reduced to 1 drop once a day in the morning. Doses exceeding 1 drop of a 0.5% solution of timolol 2 times a day do not lead to an additional decrease in intraocular pressure.If the application of timolol fails to achieve the required level of intraocular pressure, it is necessary to consider the use of additional antihypertensive drugs. The simultaneous use of two beta-blockers for local use is impossible. In patients with a significantly pigmented iris, there may be a less pronounced decrease in intraocular pressure, as well as a longer period to achieve compensation of intraocular pressure. After cessation of treatment, the hypotensive effect of timolol may persist for several days, and in the case of long-term prior treatment, the residual hypotensive effect may persist from 2 to 4 weeks. When treating with timolol only in relation to one eye, a hypotensive effect may also be noted in relation to the contralateral eye. Monitoring the effectiveness of the drug is recommended about 3-4 weeks after the start of therapy (no earlier than 1-2 weeks). With prolonged use of timolol, a weakening effect is possible. Switching from another antihypertensive therapy: When switching from therapy with one beta-blocker to another drug from the group of beta-blockers, it is recommended to complete a full day of therapy with the previously used antihypertensive agent, and start instillation of timolol 0.25% in each affected eye by 1 drop 2 times a day. In the absence of an adequate response to therapy, the dose can be increased to one drop of a 0.5% solution of timolol in each affected eye twice a day. When switching to therapy with a hypotensive drug from another group, other than beta-blockers, continue instillations of a previously prescribed drug with the addition of instillations of one drop of a 0.25% solution of timolol in each affected eye twice a day. The next day, the previous treatment is canceled and therapy with timolol continues. Use in the pediatric population According to limited data, timolol can be recommended for reducing intraocular pressure in infantile and juvenile congenital glaucoma in the preoperative period or in the case of ineffective surgical treatment.Before using the drug, it is necessary to carefully evaluate the risks and benefits of using timolol in the pediatric population by carefully collecting anamnesis for systemic disorders. In case the benefit outweighs the risk, it is recommended to use timolol in the lowest available concentration of 1 drop 1 time per day. With insufficient control of intraocular pressure, it is necessary to switch to use 2 times a day, 1 drop with an interval of 12 hours between instillations. Control of eye and systemic side effects is necessary within 1-2 hours after the first instillation, especially in newborns and children under 3 years of age, connection with the possibility of developing apnea and respiration according to the Cheyne-Stokes type. It is necessary to warn the parents of the child receiving treatment with timolol that the drug should be canceled if the child develops side effects from the respiratory system, in particular, coughing and sneezing. Treatment with Timolol is usually carried out for a long time. A break in treatment or a change in dosage of the drug is carried out only as prescribed by the attending physician.
Side effects
Adverse reactions that occur after ingestion of timolol and other beta-blockers can be regarded as potential adverse reactions and for timolol preparations in the dosage form eye drops. The adverse reactions that were obtained during clinical trials and post-marketing follow-up of timolol drugs in the dosage form of eye drops. The frequency of side effects identified both during the studies and post-tracking observation was estimated as follows: very often (≥1 / ten); often (≥1 / 100 to <1/10); sometimes (≥1 / 1000 to <1/100); rarely (≥1 / 10,000 to <1/1000); very rarely (<1/10000), the frequency is unknown (the available data cannot be estimated). General reactions With an unknown frequency: headache, asthenia / fatigue, chest pain. On the part of the organ of vision Often: blurred vision, pain in the eyes, burning and itching in the eyes, discomfort in the eye, conjunctival injection. Infrequently: blepharitis, punctate keratitis, keratitis, conjunctivitis, iritis, diplopia, corneal erosion, corneal ulcer, tearing or reduction of tearing, photophobia, feeling of "sand" in the eyes, eyelid edema, conjunctiva swelling, ptosis. Rarely: uveitis, double vision, corneal pigmentation, eyelid erythema. Very rarely: the development of corneal calcification with significant damage due to the presence of phosphates in the composition of the droplets.With an unknown frequency: decreased sensitivity of the cornea, choroid detachment in the postoperative period of antiglaucomatous surgery. Since the cardiovascular system Infrequently: bradycardia, hypotension. Rarely: myocardial infarction, decrease or increase in blood pressure, intermittent claudication. With unknown frequency: cardiac arrest, atrioventricular block, arrhythmia, rapid heartbeat, congestive heart failure, Raynaud's phenomenon. On the part of the digestive system Infrequently: dysgeusia. Rarely: dyspepsia, dryness of the oral mucosa, abdominal pain. With unknown frequency: nausea, vomiting, diarrhea. On the part of the immune system With an unknown frequency: systemic lupus erythematosus. Mental disorders Rarely: depression. With unknown frequency: insomnia, memory loss, nightmare dreams. Of the nervous system Infrequently: headache. Rarely: cerebral ischemia, dizziness, migraine. With an unknown frequency: impaired cerebral circulation, fainting, paresthesia, dizziness, aggravation of myasthenia gravis. On the part of the skin and subcutaneous tissue Rarely: swelling of the face, erythema. With unknown frequency: psoriasis or worsening of the course of psoriasis, localized rash, alopecia. On the part of the connective tissue With an unknown frequency: arthropathy, muscle pain. Allergic reactions With an unknown frequency: systemic allergic reactions, including anaphylaxis, angioedema, urticaria, local or generalized rash, pruritus. On the part of the respiratory system and mediastinal organs Infrequently: respiratory failure, shortness of breath, bronchitis. Rarely: bronchospasm (mainly in patients with already existing bronchospastic conditions), cough, nasal congestion, infections of the upper respiratory tract. On the part of the endocrine system With an unknown frequency: the subclinical course of hypoglycemia in patients with diabetes mellitus (see the section "Special Instructions"). From the genitourinary system With unknown frequency: retroperitoneal fibrosis, sexual dysfunction (including impotence), decreased libido, Peyronie's disease. On the part of ENT organs. With unknown frequency: ringing in the ears. Adverse reactions that occur after taking timolol or other beta-blockers inside Allergic reactions: erythematous rash, fever, accompanied by sore throat, laryngism, accompanied by distress syndrome.General reactions and reactions at the injection site: pain in the extremities, decrease in exercise tolerance, weight loss. Since the cardiovascular system: worsening of arterial insufficiency, vasodilation. On the part of the digestive system: gastrointestinal pain, hepatomegaly, vomiting, thrombosis of mesenteric arteries, ischemic colitis. From the side of blood and lymphatic system: net thrombocytopenic purpura, thrombocytopenic purpura, agranulocytosis. On the part of the endocrine system: hyperglycemia, hypoglycemia. On the part of the skin and subcutaneous tissues: itching, skin irritation, increased pigmentation, sweating. On the part of the musculoskeletal system: arthralgia. Nervous system / mental disorders: vertigo, decreased concentration, reversible inhibition of mental functions, progressing to catatonia, acute reversible syndrome characterized by impaired orientation in time and space, emotional lability, some difficulty in perception and reduced ability to perform neuropsychiatric tests. On the part of the respiratory system: wheezing, bronchial obstruction. From the urinary system: difficulty urinating.
Overdose
Possible development of systemic effects characteristic of beta-blockers: dizziness, headache, arrhythmia, bradycardia, bronchospasm, nausea and vomiting, loss of consciousness, hypotension, shortness of breath, generalized convulsions, cardiogenic shock, heart failure and cardiac arrest. In case of accidental ingestion of timolol, gastric lavage and ingestion of activated carbon are necessary. It is shown that the drug can not be removed from the body by hemodialysis. With the development of bradycardia and bradyarrhythmias (with atrioventricular blockade of grade II and III), intravenous administration of atropine sulfate in a dose of 0.25 to 2 mg is recommended; after partial relief of bradycardia, isoprenaline is indicated. For difficult-to-stop bradycardia, consideration should be given to installing a pacemaker. In case of hypotension, sympathomimetic drugs such as dopamine, dobutamine, norepinephrine are recommended. In the absence of effect - the introduction of glucagon. With the development of acute heart failure, the use of drugs of digitalis and diuretics, as well as oxygen therapy, with ineffectiveness, intravenous administration of aminophylline is recommended.
Interaction with other drugs
The combined use of the drug with eye drops containing adrenaline can cause pupil dilation.The specific effect of the drug is a reduction in intraocular pressure, which may increase with the simultaneous use of eye drops containing epinephrine and pilocarpine. Two different beta-blockers should not be instilled into the same eye. Hypotension and bradycardia may increase with simultaneous use of the drug with calcium antagonists, reserpine and systemic beta-blockers. CYP2D6 inhibitors, such as quinidine and cimetidine, can increase the concentration of timolol in plasma. Concomitant use with insulin or oral antidiabetic agents may result in hypoglycemia. Timolol enhances the action of muscle relaxants, therefore, it is necessary to remove the drug 48 hours before the planned surgical intervention under general anesthesia. These data may also apply to drugs that were used shortly before.
special instructions
In the postoperative period of antiglaucomatous operations and with the use of drugs that reduce the secretion of intraocular fluid, the development of choroidal detachment is possible. The use of timolol in patients with atopy or severe pathological reactions to various allergens in the history can provoke more severe reactions in response to accidental, diagnostic or therapeutic management of allergens. Such patients may respond poorly to the administration of conventional doses of epinephrine to relieve anaphylactic reactions. Beta-blockers are able to mask a number of clinical symptoms of hyperthyroidism (in particular tachycardia). Care is required when using beta-blockers in patients with the possibility of thyrotoxicosis. In patients with a history of heart failure, prolonged myocardial depression in some cases can lead to the development of heart failure. At occurrence of the first signs of heart failure, timolol should be canceled. Care must be taken in the appointment of timolol in patients with atrioventricular block I degree, Prinzmetal angina pectoris and peripheral circulatory disorders (Raynaud's phenomenon). The main pathogenetic aspect of the treatment of angle-closure glaucoma is the need to open the anterior chamber angle, which is achieved by constricting the pupil with the help of miotics. In connection with the absence of the effect of timolol on the diameter of the pupil in the treatment of angle-closure glaucoma, the drug can be used only in combination with miotics.Because of the possible effect of beta-adrenoreceptor blockers on blood pressure and the number of heartbeats, these drugs should be used with caution in patients with cerebrovascular insufficiency. If, after initiating therapy with timolol, signs or symptoms of decreased cerebral circulation develop, the need for therapy with local beta-blockers should be reconsidered. The use of timolol may increase muscle weakness in myasthenia gravis (for example, cause increased diplopia, ptosis and general weakness). In some patients with myasthenia gravis and other myasthenic diseases, an increase in muscle weakness was observed with timolol. With simultaneous use with other drugs, it is necessary to observe the interval between instillations of at least 15 minutes. When applied, it is necessary to monitor the tearing function, the state of the cornea, and to evaluate the size of the visual fields at least 1 time in 6 months. The drug contains preservative benzalkonium chloride, which can cause eye irritation, be absorbed by soft contact lenses, causing a change in their color and have an adverse effect on eye tissue. Contact lenses should be removed before using the drug and, if necessary, wear them again no earlier than 15 minutes after instillation. With prolonged use of the drug, the toxic effect of the preservative benzalkonium chloride on the corneal epithelium (the development of punctate keratopathy and / or toxic ulcerative keratopathy) is possible. Cases of the development of bacterial keratitis in patients who used timolol in containers for multiple dosing of ophthalmic drugs have been noted. These containers were inadvertently contaminated with patients with concomitant corneal diseases. When transferring patients to treatment with timolol, correction of refraction changes caused by previously applied myotics may be necessary. The drug, like other beta-blockers, can hide the possible symptoms of hypoglycemia in the blood of patients with diabetes mellitus. In the case of the upcoming surgery under general anesthesia, it is necessary to cancel the drug 48 hours before the operation, as it enhances the action of muscle relaxants and general anesthetics.