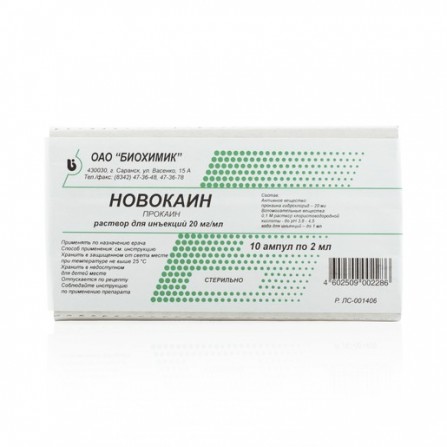
Novocaine injection for 2% ampoules 2 ml 10 pcs
Condition: New product
999 Items
Rating:
Be the first to write a review!

More info
Active ingredients
Procaine
Release form
Solution
Composition
1 ml of drops contains 6.8 mg of timolol maleate (5 mg of timolol). Excipients: benzalkonium chloride; sodium dihydrogen phosphate monohydrate; phosphate dodecahydrate disodium; sodium chloride; edetate dihydrate disodium; sodium hydroxide; purified water
Pharmacological effect
Local anesthetic with moderate activity and a wide range of therapeutic actions. When administered intravenously, it has analgesic and anti-shock activity, hypotensive and antiarrhythmic action. It prevents the generation of impulses in the endings of sensory nerves and conduction of impulses along the nerve fibers. Changes the action potential in the membranes of nerve cells without a pronounced effect on the resting potential. During absorption and direct vascular injection into the blood stream, it reduces the excitability of peripheral cholinergic systems, reduces the formation and release of acetylcholine from preganglionic endings, reduces spasm of smooth muscles, and inhibits the excitability of the myocardium and motor cortex of the brain. Eliminates the downward inhibitory effects of the reticular formation of the brain stem. Inhibits polysynaptic reflexes. In large doses, it can disrupt the neuromuscular conduction and cause convulsions. Shows a short anesthetic activity (duration of infiltration anesthesia is 0.5–1 h). Compared with lidocaine and buvicain, procaine has a less pronounced anesthetic effect, and therefore has relatively low toxicity and a greater therapeutic latitude. Antiarrhythmic effect due to an increase in the refractory period, a decrease in excitability and automatism of the myocardium. When administered intramuscularly effective for the treatment of elderly patients in the early stages of diseases associated with functional disorders of the central nervous system
Pharmacokinetics
When administered parenterally well absorbed. The degree of absorption depends on the place and route of administration (especially on vascularization and blood flow velocity in the area of administration) and the final dose (amount and concentration). It is rapidly hydrolyzed by plasma and tissue esterases and cholinesterases to form two main pharmacologically active metabolites: diethylaminoethanol (it hasmoderate vasodilating action) and para-aminobenzoic acid (is a competitive antagonist of sulfanilamide chemotherapeutic drugs and may weaken their antimicrobial action). The half-life is 30–50 s, in the neonatal period - 54–114 s. Excreted mainly by the kidneys in the form of metabolites (80%); in unchanged form is displayed no more than 2%. Metabolism of procaine is impaired in patients with genetic insufficiency of plasma cholinesterase. Poorly absorbed through mucous membranes
Indications
Infiltration, conduction, epidural and spinal anesthesia; vagosympathetic and perirenal blockade; pain in gastric ulcer and duodenal ulcer, hemorrhoids, nausea
Contraindications
Individual sensitivity
Precautionary measures
Before using procaine, it is mandatory to have a skin test for individual sensitivity to the drug, as indicated by edema and redness of the injection site. When using the drug, it is necessary to control the functions of the cardiovascular, respiratory and central nervous systems. To reduce the systemic effect, toxicity and prolongation of the effect during local anesthesia, procaine is used in combination with vasoconstrictors (0.1% solution of epinephrine hydrochloride at the rate of 1 drop per 2–5 ml of solution of novocaine). When conducting local anesthesia with the use of the same total dose, the toxicity of procaine is the higher, the more concentrated is the solution used. In this regard, with an increase in the concentration of the solution, the total dose is recommended to reduce or dilute the drug solution to a lower concentration (sterile isotonic sodium chloride solution). To prevent the development of hypersensitivity reactions, therapy begins with the introduction of 2 ml of 2% solution after 3 days (in the absence of side effects ) enter 3 ml, then proceed to the introduction of a full dose - 5 ml per injection. The drug is used with caution in emergency operations, accompanied by acute blood loss, conditions accompanied a decrease in hepatic blood flow, progression of cardiovascular insufficiency (usually due to the development of heart blocks and shock), inflammatory diseases or infection of the injection site, deficiency of pseudocholinesterase, renal failure,children (up to 18 years), in elderly patients (over 65), seriously ill, debilitated patients, during pregnancy, during childbirth and lactation (breastfeeding) Procaine slowly penetrates the intact mucous membranes, as a result of which it does not provide surface anesthesia. the period of outpatient treatment is necessary to refrain from driving and performing work that requires increased attention, speed of mental and motor reactions
Use during pregnancy and lactation
In pregnancy and lactation, the drug is used only if the benefit to the mother outweighs the potential risk to the fetus and child.
Dosage and administration
Novocaine is administered intramuscularly - 5-10 ml of 1-2% solution 3 times a week for a month, after which a 10-day break is taken; 0.25-0.5% solutions are used for infiltration anesthesia, and 2% solution for conduction anesthesia. Inside - 1/2 tsp (with pain).
Dosage and administration
. Novocaine is used intracutaneously, intramuscularly, intravenously. For infiltration anesthesia, a 0.25–0.5% solution is used, for anesthesia using the Vishnevsky method (tight creeping infiltration), 0.125–0.25% solutions, for conduction anesthesia, 1–2% solutions, for epi- or epidural anesthesia - 2% solution. Possible appointment for intraosseous anesthesia. If it is necessary to use lower concentrations of procaine (0.125% or 0.25%), dilute the solutions with sterile isotonic sodium chloride solution before use. Intravenous administration is carried out slowly, better in an isotonic solution of sodium chloride. With local anesthesia, the dosing regimen is individual, depending on the type of anesthesia, route of administration, indications, condition and age of the patient. For conduction anesthesia, up to 25 ml of a 2% solution is injected; for epidural - 20–25 ml of 2% solution. Higher doses of procaine with a conductive blockade of nerves and plexuses, epidural anesthesia - not more than 0.5 g once without epinephrine or 1 g with epinephrine. In case of perirenal blockade (according to Vishnevsky), 50–80 ml of 0.5% solution is injected into the kidney cellulose tissue, and 30–100 ml of 0.25% solution in the vagosympathetic blockade. To relieve pain syndrome is used intramuscularly or intravenously.Intravenously administered from 1 ml to 10-15 ml of 0.5% solution. For circulatory and paravertebral blockade with eczema and neurodermatitis, novocaine 0.5% is used intracutaneously. For the treatment of early stages of diseases that are more common in the elderly (endarteritis, atherosclerosis, arterial hypertension, spasms of the coronary vessels and brain vessels, diseases of rheumatic and infectious origin, etc.) are injected intramuscularly with a 2% solution of 5 ml 2 times a week, the course - 12 injections, a break - 10 days (four courses are possible within a year). When atrial fibrillation is administered intravenously, a 0.25% solution of 2–4 ml 4–5 times a day. For adults, the maximum single dose for intramuscular injection - 0.1 g, intravenous - 0.05 g; maximum daily doses for both routes of administration - 0.1 g. Doses for children, depending on age and body weight, have not been developed. Novocaine is also used to dissolve the antibiotics of the penicillin group in order to prolong their action.Side effects
Dizziness, weakness, hypotension, allergic reactions
Overdose
Symptoms: pallor of the skin and mucous membranes, dizziness, nausea, vomiting, increased nervous irritability, cold sweat, tachycardia, decrease in blood pressure to almost collapse, tremor, convulsions, apnea, methemogoglobinemia, respiratory depression, sudden heart failure, heart failure. The effect on the central nervous system is manifested by a sense of fear, hallucinations, convulsions, motor agitation. In cases of overdose, administration of the drug should be immediately discontinued. When conducting local anesthesia, the site of injection can be crushed with adrenaline. Treatment: general resuscitation measures, which include inhalation of oxygen, if necessary, carrying out artificial ventilation of the lungs. If convulsions last more than 15–20 sec, they are stopped by intravenous administration of thiopental (100–150 mg) or diazepam (5–20 mg). In case of arterial hypotension and / or depression of the myocardium, ephedrine (15-30 mg) is injected intravenously, in severe cases, detoxification and symptomatic therapy. In the event of intoxication after injection of novocaine into the muscles of the leg or arm, an urgent application of the harness is recommended to reduce the subsequent flow of the drug into the general bloodstream.
Interaction with other drugs
Prolongs the neuromuscular blockade caused by suxametonium (since both drugs are hydrolyzed by plasma cholinesterase). Concurrent use with MAO inhibitors (furazolidone, procarbazine, selegolin) increases the risk of arterial hypotension. Toxicity of procain increases anticholinesterase drugs (suppressing its hydrolysis). The procaine metabolite (para-aminobenzoic acid) is a competitive antagonist of sulfanilamide drugs and may impair their antimicrobial action. When processing the injection site of a local anesthetic with disinfectant solutions containing heavy metals, the risk of developing a local reaction in the form of pain and swelling increases. Potentiates the effect of direct anticoagulants. The drug reduces the effect of anticholinesterase drugs on neuromuscular transmission. Cross-sensitization possible
special instructions
With caution: in violation of the function of the cardiovascular system; with heart failure