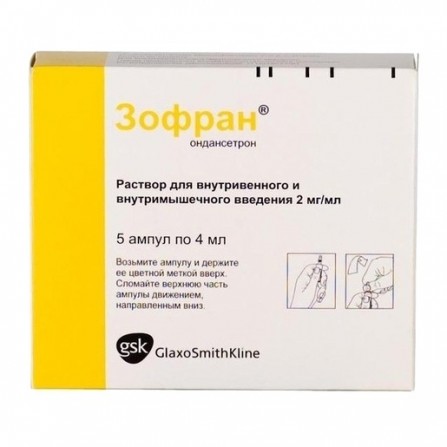
Zofran injection solution 2mg ml ampoule 4ml N5
Condition: New product
1000 Items
Rating:
Be the first to write a review!

More info
Active ingredients
Ondansetron
Composition
Ondansetron hydrochloride dihydrate 5 mg, which corresponds to the content of Ondansetron 4 mg. Excipients: citric acid monohydrate, sodium citrate, Sodium chloride, water d / and.
Pharmacological effect
Antiemetic drug, selective serotonin 5HT3 receptor antagonist. Ondansetron is a potent, highly selective antagonist of 5HT3 receptors. The mechanism for suppressing nausea and vomiting is not precisely known. With radiation therapy and the use of chemotherapeutic drugs, serotonin (5HT) may be released in the small intestine, causing an emetic reflex through activation of 5HT3 receptors and stimulation of the afferent endings of the vagus nerve. Ondansetron blocks the initiation of this reflex. Activation of the afferent endings of the vagus nerve, in turn, can cause the release of 5HT in the posterior field of the fourth ventricle (area postrema), and, therefore, trigger the gag reflex through the central mechanism. Thus, the action of ondansetron on suppressing nausea and vomiting triggered by cytotoxic chemotherapy and radiotherapy is likely due to the antagonistic effect on the 5HT3 receptors of neurons located both in the periphery and in the central nervous system. The mechanism of action of the drug in the management of postoperative nausea and vomiting is unclear, probably it is similar to that in the management of chemo-and radio-induced nausea and vomiting. Ondansetron does not affect the concentration of prolactin in the blood plasma.
Pharmacokinetics
The pharmacokinetic parameters of ondansetron do not change with its repeated administration. Absorption Ondansetron has the same systemic effects when in / m and / in the introduction. Distribution Ondansetron has a moderate ability to bind to plasma proteins (70-76%). The distribution of ondansetron is similar when IM and IV injection in adults. Vd in equilibrium is about 140 liters. Metabolism Ondansetron is metabolized mainly in the liver with the participation of several enzymes. The absence of CYP2D6 enzyme (sparteine / debrisoquine type polymorphism) does not affect the pharmacokinetics of ondansetron. Withdrawal Ondansetron is derived from systemic blood flow, mainly through metabolism in the liver. Less than 5% of the administered dose is excreted unchanged in the urine.T1 / 2 of ondansetron, both after i / m and after iv administration, is approximately 3 hours. Pharmacokinetics in special clinical situations The pharmacokinetics of ondansetron depends on the gender of the patients. Women have lower systemic clearance and Vd (figures adjusted for body weight) than men. In a clinical study, children aged 1 to 24 months (51 patients) received ondansetron at a dose of 0.1 mg / kg or 0.2 mg / kg before surgery. In patients aged 1 to 4 months, clearance was approximately 30% less than in patients aged 5 to 24 months, but is comparable with this indicator in patients aged 3 to 12 years (with correction of indicators depending on weight body). T1 / 2 in the group of patients at the age of 1–4 m averaged 6.7 h; in the age groups 5–24 months and 3–12 years, 2.9 hours. In patients aged 1–4 months, dose adjustment is not required, since a single IV administration of ondansetron is used to treat postoperative nausea and vomiting in this category of patients. The differences in pharmacokinetic parameters are partly due to higher Vd in patients aged 1 to 4 months. In a study of children aged 3–12 years (21 patients) who underwent planned surgical interventions under general anesthesia, the absolute values of clearance and Vd of ondansetron after a single intravenous dose of 2 mg (from 3 to 7 years) or 4 mg ( from 8 to 12 years) were reduced in comparison with values in adults. Both parameters increased linearly depending on body weight, in patients aged 12 years, these values approached the values in adults. When correcting the values of clearance and Vd, depending on body weight, these parameters were close in different age groups. Dose calculation based on body weight (0.1 mg / kg, up to a maximum of 4 mg) compensates for these changes and the systemic exposure of ondansetron in children. A population-based pharmacokinetic analysis was carried out in 74 patients aged from 6 to 48 months who were given IV ondansetron at a dose of 0.15 mg / kg every 4 hours in the amount of 3 doses to relieve nausea and vomiting caused by chemotherapy, and in 41 patients aged from 1 to 24 months after surgical interventions, which were administered ondansetron in a single dose of 0.1 mg / kg or 0.2 mg / kg. Based on the pharmacokinetic parameters of this group for patients aged 1 to 48 months, administration of ondansetron IV dose of 0.15 mg / kg every 4 hours in an amount of 3 doses should lead to a systemic exposure (AUC) comparable to that ofwhich is observed when using the drug in the same doses in children aged 5 to 24 months with surgical interventions, as well as in previous studies in children with oncological diseases (aged 4 to 18 years) and during surgical intervention (from the age of 3 up to 12 years). Studies conducted in elderly patients have shown a weak, clinically insignificant, age-dependent increase in T1 / 2 of ondansetron. In patients with moderately impaired renal function (creatinine clearance 15-60 ml / min) with on / in ondansetron administration, both systemic clearance and ondansetron Vd are reduced, resulting in a small and clinically insignificant increase in its T1 / 2 (to 5.4 hours) . The pharmacokinetics of ondansetron during its intravenous administration remained almost unchanged in patients with severe renal dysfunction on chronic hemodialysis (the studies were conducted in the intervals between hemodialysis sessions). In patients with severely impaired liver function, systemic clearance of ondansetron is sharply reduced with an increase in T1 / 2 to 15-32 h.
Indications
- prevention and elimination of nausea and vomiting caused by cytotoxic chemotherapy or radiotherapy; - prevention and elimination of postoperative nausea and vomiting.
Contraindications
- pregnancy; - lactation (breastfeeding); - hypersensitivity to the drug. The drug should be used with caution in patients with cardiac rhythm and conduction disturbances, patients receiving antiarrhythmic drugs and beta-blockers, and patients with significant electrolyte disturbances (very rarely, transient ECG changes, including prolongation of the QT interval, have been reported with IV injection of Zofran).
Use during pregnancy and lactation
The drug is contraindicated for use during pregnancy and lactation (breastfeeding).
Dosage and administration
Nausea and vomiting caused by chemotherapy and / or radiotherapy. The choice of dosing regimen is determined by the emethogenicity of antitumor therapy. Adults In case of moderate emetogenic chemotherapy or radiotherapy, the drug is administered in a dose of 8 mg IV (slowly) or IM immediately before the start of chemotherapy or radiotherapy.Patients receiving highly emethogenic chemotherapy, for example, cisplatin in high doses, Zofran can be prescribed as a single intravenous or intramuscular injection at a dose of 8 mg just before chemotherapy. Zofran in a dose of 8 mg to 32 mg should be administered only by iv infusion after dissolving the drug in 50-100 ml of a 0.9% solution of sodium chloride or in another compatible infusion solution for 15 minutes or more. Another way is to administer Zofran in a dose of 8 mg slowly in / in or intramuscularly immediately before chemotherapy with the subsequent appointment of two injections of the drug in / in or intramuscularly in a dose of 8 mg with an interval of 2-4 hours or using a constant infusion of the drug with at a rate of 1 mg / h for 24 hours. In the case of highly emitting antitumor therapy, the effectiveness of Zofran can be enhanced by an additional single IV injection of dexamethasone sodium phosphate at a dose of 20 mg before the start of chemotherapy. Zofran oral or rectal dosage forms are recommended to prevent delayed or continuing vomiting after the first day after chemotherapy. Children and adolescents aged from 6 months to 17 years. Children with a surface area of less than 0.6 m2 initial dose of 5 mg / m2 is injected into / in immediately before chemotherapy, followed by taking Zofran orally at a dose of 2 mg (in the form of syrup) after 12 hours. Within 5 days after the course of treatment, therapy is continued, taking Zofran orally at a dose of 2 mg 2 times / day. Children with a body surface area of 0.6-1.2 m2 Zofran is administered intravenously once in a dose of 5 mg / m2 immediately before chemotherapy, followed by taking the drug orally at a dose of 4 mg after 12 hours. Reception of Zofran orally at a dose of 4 mg 2 times / day can be continued for 5 more days after the course of chemotherapy. For children with a body surface area of more than 1.2 m2, an initial dose of 8 mg is given in / immediately before chemotherapy, followed by taking the drug orally at a dose of 8 mg after 12 hours. Oral administration of Zofran orally at a dose of 8 mg 2 times / day can be continued even within 5 days after the course of chemotherapy. As an alternative to children aged 6 months and older, Zofran is administered intravenously once at a dose of 0.15 mg / kg (not more than 8 mg) immediately prior to chemotherapy. This dose can be re-administered every 4 hours, for a total of no more than three doses in total.Intake of Zofran orally at a dose of 4 mg 2 times / day can be continued for another 5 days after the course of chemotherapy. Doses should not exceed the recommended for adults. Other categories of patients In elderly patients, dose adjustment of Zofran is not required. Patients with impaired renal function dose adjustment Zofran not required. In cases of impaired liver function, the clearance of ondansetron is significantly reduced, T1 / 2 is increased in patients with impaired liver function of moderate and severe degree. The daily dose of Zofran should not exceed 8 mg. In patients with a slower metabolism of spartein and debrisoquine T1 / 2 ondansetron is not changed. Consequently, upon repeated administration of Zofran, its concentration in plasma will not differ from that in the general population. Therefore, these patients do not require correction of the daily dose or the frequency of receiving ondansetron. Nausea and vomiting in the postoperative period. Adults To prevent nausea and vomiting in the postoperative period, a single IM or a slow intravenous Zofran injection at a dose of 4 mg is recommended during induction of anesthesia. For the treatment of nausea and vomiting in the postoperative period, Zofran is administered once at a dose of 4 mg IM or slowly IV. Children and adolescents aged 1 month to 17 years To prevent nausea and vomiting in the postoperative period in children undergoing surgery under general anesthesia, Zofran can be administered at a dose of 0.1 mg / kg (up to 4 mg) as a slow IV injection before, during or after induction of anesthesia or after surgery. For the relief of nausea and vomiting that developed in the postoperative period, a slow intravenous injection of Zofran at a dose of 0.1 mg / kg (maximum up to 4 mg) is recommended. Other patient categories There is limited experience with Zofran for the prevention and relief of postoperative nausea and vomiting in elderly patients, although Zofran is well tolerated by patients over 65 years of age who receive chemotherapy. Patients with impaired renal function dose adjustment Zofran not required. In cases of impaired liver function, the clearance of ondansetron is significantly reduced, T1 / 2 is increased in patients with impaired liver function of moderate and severe degree. The daily dose of Zofran should not exceed 8 mg.Patients with a slow metabolism of spartein / debrisoquine In patients with a slow metabolism of sparteine and debrisoquine T1 / 2, ondansetron is not changed. Consequently, upon repeated administration of Zofran, its concentration in plasma will not differ from that in the general population. Therefore, these patients do not require correction of the daily dose or the frequency of receiving ondansetron. Rules for the preparation of solutions and use of the drug For dilution of the injection solution, the following solutions can be applied: 0.9% sodium chloride solution, 5% dextrose solution, Ringer's solution, 10% mannitol solution, 0.3% potassium chloride solution and 0.9% sodium chloride solution, 0.3% potassium solution chloride and 5% dextrose solution. Infusion solution should be prepared immediately before use. If necessary, the finished infusion solution can be stored until use for a maximum of 24 hours at a temperature from 2 ° to 8 ° C. No protection from light is required during the infusion; the diluted injection solution maintains its stability for at least 24 hours in natural light or normal light.
Side effects
Determination of the frequency of adverse reactions: very often (1/10), often (1/100 and <1/10), sometimes (1/1000 and <1/100), rarely (1/10 000 and <1/1000), very rarely (<1/10 000), including individual messages. Allergic reactions: rarely - immediate type hypersensitivity reactions, in some cases severe, including anaphylaxis. From the nervous system: very often - a headache; sometimes - convulsions, movement disorders (including extrapyramidal symptoms, such as dystonia, ocular curvature / eye cramps / and dyskinesia) in the absence of persistent clinical consequences; rarely - dizziness during rapid on / in the introduction. On the part of the organ of vision: rarely - transient visual disturbances (blurred vision), mainly during i.v. administration; very rarely, transient blindness, mainly during intravenous administration. Most cases of blindness were resolved safely within 20 minutes. Most patients received chemotherapy drugs containing cisplatin. In some cases, transient blindness was of cortical genesis. Since the cardiovascular system: sometimes - arrhythmia, chest pain, as accompanied, and not accompanied by a decrease in the ST segment, bradycardia, decrease in blood pressure; often - feeling hot or flushing; very rarely, transient ECG changes, including prolongation of the QT interval, mainly when intravenously administered.On the part of the digestive system: often - constipation; sometimes an asymptomatic increase in liver function tests (mainly observed in patients receiving chemotherapy with cisplatin). Local reactions: often - local reactions at the site of intravenous injection. Other: sometimes - hiccups.
Overdose
Currently, there is little data on the overdose of ondansetron. Symptoms: in most of the observed cases, the symptoms of overdose coincided with adverse reactions that occur when taking the drug Zofran in the recommended doses. Treatment: there is no specific antidote for Zofran, therefore, if an overdose is suspected, symptomatic and supportive therapy is recommended.
Interaction with other drugs
There is no evidence that ondansetron induces or inhibits the metabolism of other drugs, often prescribed in combination with it. According to special studies found that ondansetron does not interact with ethanol, temazepam, furosemide, tramadol and propofol. Ondansetron is metabolized by several isoenzymes of the cytochrome P450 system (CYP3A4, CYP2D6 and CYP1A2). Due to the variety of isoenzymes that can metabolize ondansetron, inhibition of isoenzymes or a decrease in the activity of one of the isoenzymes (for example, genetic deficiency of CYP2D6) is usually compensated by other isoenzymes, as a result of which changes in the overall clearance of ondansetron are absent or insignificant and do not require dose adjustment. In patients receiving potent inducers of CYP3A4 (phenytoin, carbamazepine and rifampicin), the concentration of ondancentron in the blood was low. There is evidence from small studies suggesting that ondansetron may reduce the analgesic effect of tramadol. Pharmaceutical interaction Zofran at a concentration of 16 µg / ml and 160 µg / ml (which corresponds to 8 mg / 500 ml and 8 mg / 50 ml, respectively) is pharmaceutically compatible and can be administered via a Y-shaped injector in / in a drip together with the following drugs: - cisplatin (at a concentration of up to 0.48 mg / ml) for 1-8 hours; - 5-fluorouracil (at a concentration of up to 0.8 mg / ml at a rate of 20 ml / h - higher concentrations of 5-fluorouracil may cause precipitation of Zofran); - carboplatin (at a concentration of 0.18-9.9 mg / ml) for 10-60 minutes; - etoposide (at a concentration of 0.144-025 mg / ml for 30-60 minutes); - ceftazidime (at a dose of 0.25-2 g,in the form of iv bolus injection for 5 min); - cyclophosphamide (at a dose of 0.1-1 g, in the form of iv bolus injection for 5 min); - doxorubicin (in a dose of 10-100 mg, in the form of intravenous bolus injection for 5 minutes); - dexamethasone (possibly in / in the introduction of 20 mg of dexamethasone slowly over 2-5 minutes). Drugs can be administered through a single dropper, while the concentration of dexamethasone sodium phosphate in the solution can be from 32 μg to 2.5 mg / ml, Zofran - from 8 μg to 1 mg / ml.
special instructions
There are reports of the occurrence of hypersensitivity reactions to ondansetron in patients with a history of increased sensitivity to other selective antagonists of 5HT3 receptors. Since it is known that ondansetron increases the time it takes for the contents to pass through the large intestine, in case of using the drug in patients with symptoms of subacute intestinal obstruction, regular monitoring is necessary. Zofran should not be administered in the same syringe or in the same infusion solution with other drugs. Use in Pediatrics Currently, there are limited data ondansetron use in children under the age of 1 month. Influence on the ability to drive vehicles and control mechanisms Zofran does not have a sedative effect and does not affect the ability of patients to drive vehicles or engage in other potentially dangerous activities that require increased concentration of attention and speed of psychomotor reactions.